Insulin resistance and diabetes are two separate conditions that are often confused with each other. Insulin resistance is a condition in which the body becomes resistant to insulin, while diabetes is a metabolic disorder characterized by high blood sugar levels.
What is insulin resistance?
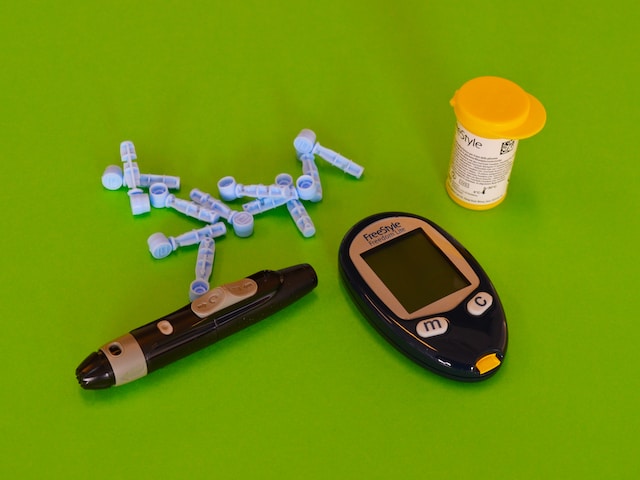
(Photo by Mykenzie Johnson on Unsplash )

Insulin resistance is a metabolic disorder that affects how the body processes glucose, leading to high blood sugar levels. It occurs when cells in the muscles, liver and fat become less responsive to insulin hormone produced by the pancreas. Insulin is essential for transporting glucose from the bloodstream into cells where it can be used as energy or stored as glycogen.
When there’s too much glucose circulating in your blood, your pancreas produces more insulin to try to lower it. However, over time, this leads to an excess of insulin in your bloodstream which further contributes to insulin resistance.
Several factors contribute to developing insulin resistance including genetics, obesity, physical inactivity and unhealthy eating habits. People with type 2 diabetes are often diagnosed with underlying insulin resistance before their condition worsens.
The diagnosis of insulin resistance usually involves measuring fasting glucose levels and performing a test called oral glucose tolerance test (OGTT). Treatment options include lifestyle modifications such as losing weight through exercise and healthy diet or medications such as metformin that improves sensitivity towards insulin.
What is diabetes?

Diabetes is a chronic condition that affects millions of people worldwide. It occurs when the body either doesn’t produce enough insulin or can’t effectively use the insulin it produces. Insulin is a hormone produced by the pancreas, which helps regulate blood sugar levels. Without enough insulin, glucose accumulates in the bloodstream instead of entering cells to be used for energy.
There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disease that typically develops in childhood or adolescence when the immune system attacks and destroys pancreatic cells that produce insulin. Type 2 diabetes usually develops later in life and is often associated with lifestyle factors such as obesity, poor diet, and lack of exercise.
In addition to these two main types, there are also other less common forms of diabetes, including gestational diabetes (which occurs during pregnancy) and monogenic diabetes (caused by genetic mutations).
Regardless of the type, uncontrolled high blood sugar levels over time can lead to serious complications such as nerve damage, kidney failure, blindness, heart disease and stroke.
If you suspect you may have symptoms related to Diabetes consult your doctor right away for proper diagnosis and treatment options available for your specific needs.
Insulin resistance Vs. Diabetes – Key differences
Insulin resistance and diabetes are two distinct conditions, but they share some similarities. Insulin is a hormone produced by the pancreas that regulates blood sugar levels in the body. The key difference between insulin resistance and diabetes is their relationship to insulin.
Insulin resistance occurs when the cells of your body become resistant to insulin’s effects, meaning that they require more insulin than usual to achieve the same effect. This condition often precedes type 2 diabetes, as it can lead to elevated blood glucose levels over time.
Diabetes, on the other hand, occurs when your body doesn’t produce enough insulin (type 1) or can’t use it effectively (type 2). This leads to high blood sugar levels that can damage various organs and tissues in your body.
While both conditions involve issues with how the body utilizes insulin, there are some significant differences between them. Insulin resistance typically occurs before developing type 2 diabetes and may be reversible with lifestyle changes such as diet and exercise. In contrast, type 1 diabetes requires daily injections of insulin for life since the pancreas cannot produce this hormone at all.
While both conditions involve problems related to insulin utilization within our bodies – one being an early warning sign for another – they have different causes/etiologies and management approaches
Causes of insulin resistance and diabetes
Insulin resistance and diabetes share some common causes, but insulin resistance can also occur on its own. Obesity is a major risk factor for both conditions as it leads to inflammation and metabolic dysfunction. Genetics also play a role in the development of these conditions.
One of the main contributors to insulin resistance is an unhealthy diet high in refined carbohydrates and sugar. This type of diet can cause spikes in blood sugar levels, leading to increased insulin production by the pancreas over time.
Other lifestyle factors that contribute to insulin resistance include lack of exercise, poor sleep habits, chronic stress, and smoking. These factors all increase inflammation within the body which can impair insulin sensitivity.
Diabetes has additional causes including autoimmune disorders that destroy pancreatic cells responsible for producing insulin (Type 1 Diabetes) or excess fat deposits in organs such as liver or pancreas which interfere with normal glucose regulation (Type 2 Diabetes).
It’s important to note that while genetics may predispose individuals to developing these conditions, lifestyle choices are still crucial for prevention and management. Making changes like eating a healthy diet low in processed foods, getting regular exercise, reducing stress levels through mindfulness practices like yoga or meditation among others will go a long way towards preventing or managing these chronic diseases.
Symptoms of insulin resistance and diabetes
Insulin resistance and diabetes can present various symptoms that can affect your overall health. Insulin resistance is usually asymptomatic in its early stages, but as it progresses, you may experience some signs such as fatigue, brain fog, increased thirst or hunger, blurred vision and frequent urination.
On the other hand, diabetes also presents similar symptoms to insulin resistance but with some additional ones. These include weight loss (despite an increase in appetite), slow healing of wounds and infections, tingling or numbness in hands or feet and persistent skin conditions like acanthosis nigricans.
It’s essential to note that these symptoms may vary from person to person depending on a variety of factors such as age and lifestyle habits. Therefore if you feel any unease about your body’s functioning or notice any unusual changes within yourself seek medical attention immediately as it could be indicative of more severe underlying issues.
Treatment for insulin resistance and diabetes
The treatment for insulin resistance and diabetes varies based on the severity of the condition. In many cases, lifestyle changes can help manage both conditions.
For individuals with insulin resistance, losing weight through diet and exercise is often recommended to improve insulin sensitivity. Eating a balanced diet rich in whole grains, fruits, vegetables, lean proteins and healthy fats can also help.
For those with type 2 diabetes or severe insulin resistance that cannot be managed by lifestyle changes alone, medication may be necessary. Medications such as metformin work to reduce glucose production in the liver and improve insulin sensitivity.
Individuals with type 1 diabetes require daily injections of insulin to regulate their blood sugar levels since their body does not produce enough (or any) natural insulin. There are different types of insulins available depending on an individual’s needs and preferences.
In addition to medication management, regular monitoring of blood sugar levels is important for both conditions. Frequent check-ins with a healthcare provider are also essential in managing these conditions effectively.
It’s important for individuals with either condition to have a personalized treatment plan tailored to their specific needs. Collaboration between healthcare providers and patients can lead to better outcomes in managing both insulin resistance and diabetes.
Prevention of insulin resistance and diabetes
Prevention is always better than cure, and this saying holds true for insulin resistance and diabetes. The lifestyle changes that one makes can play a significant role in preventing these conditions.
Maintaining a healthy weight is crucial as obesity increases the risk of developing insulin resistance and type 2 diabetes. A balanced diet with more whole grains, fruits, vegetables, lean protein sources and less sugar and processed foods can reduce body fat accumulation.
Regular physical activity also plays an important role in preventing these conditions. Exercise helps to burn calories, manage weight loss or maintenance while improving insulin sensitivity.
Reducing stress levels through meditation or relaxation techniques may help prevent insulin resistance by reducing cortisol production – the hormone responsible for blood glucose increase during periods of stress.
Avoiding smoking and limiting alcohol consumption are other ways to prevent these conditions from occurring because both habits have been linked with increased risks of developing type 2 diabetes.
Prevention strategies are essential when it comes to managing insulin resistance and diabetes effectively. By adopting a healthier lifestyle which includes regular exercise, a balanced diet rich in fiber-rich foods supplemented with low-fat proteins while avoiding unhealthy habits like smoking; you can significantly decrease your chances of developing either condition.
Featured Image By – Diabetesmagazijn.nl on Unsplash